We are focused on delivering a clinically relevant, patient centred quality improvement programme for our local stroke and neurorehabilitation pathways of care. Given the ongoing financial challenges in health and social care, we have shifted emphasis to improvements that are cost saving or neutral, or require limited new resource. The “low hanging fruit” often centres on upskilling and training staff, improving communication and information sharing between teams and/or patients or adapting ways of work to improve efficiency.

Our portfolio of projects is diverse and covers the whole patient journey for stroke as well as community and longer-term support for neurorehabilitation.
To find out more about our projects or their impacts, get in touch with the relevant Facilitator who will be happy to provide further information.
Active projects (updated August 2025)
We have a number of paused projects that are part of wider work led by the Greater Manchester Integrated Care Board e.g. wheelchairs, seating, splinting, lycra & orthotics. It is likely these will resume when the system is ready to move forward.
Note: Hannah Jones will be on maternity leave from 6th March and her projects will be picked up by Gemma Smith who returns from maternity leave on 29th April.
| Project title | Objective(s) | Facilitator | Reports to | Projected end date |
| CVD prevention | ||||
| Atrial Fibrillation (AF) monitoring: ePatch pilot | Support pilot of ECG devices in Stepping Hill HASU to monitor for AF in stroke/TIA patients | Chris Ashton | Stroke Inpatient & Community Forum | 31/12/25 |
| Urgent care | ||||
| Pre-hospital pathway | Review updated pathway with NWAS to identify and implement improvements | Chris Ashton | HASU Forum | 31/12/25 |
| Imaging | Support implementation of national imaging pathway for stroke including roll out of CT Perfusion and rapid MR at HASUs | Chris Ashton | HASU Forum | 31/12/25 |
| Thrombolysis | Improve intervention rates at HASUs using TASC toolkit. Implement tenectoplase | Chris Ashton | HASU Forum | Ongoing |
| Acute care | ||||
| One response NWAS EPR | Make access available at all HASUs | Chris Ashton | HASU Forum | 31/12/25 |
| Patient Pass | Implement online system to improve stroke referral management across system | Chris Ashton | Stroke Inpatient & Community Forum | 31/09/25 |
| WWL stroke pathway | Support WWL to improve patient flow and access to inpatient rehabilitation | Sarah Rickard | Board | 2026 |
| MFT stroke pathway | Support MFT in developing its stroke service across the Trust, improving access to stroke care for patients at Wythenshawe | Sarah Rickard | Board | 2026 |
| Rehabilitation | ||||
| Cardiorespiratory training | Support implementation of the National Clinical Guideline for Stroke recommendation to improve health and reduce the risk of secondary CVD. | Gemma Smith | Rehabilitation Subgroup | 31/3/26 |
| Facial rehabilitation | Improve access to appropriate services in GM. Scope extent of project | Farheen Akhtar | Rehabilitation Subgroup | 31/3/26 |
| Functional Neurological Disorder (FND) | Improve equity of access to community services. Upskill GM workforce. Audit services to inform future improvement work | Gemma Smith | NR Inpatient & Community Forum | 31/3/26 |
| Increasing intensity and frequency of rehabilitation | Support teams in delivering increased rehabilitation through: digital health technologies, accessing community/voluntary sector, workforce/training & education, self management, semi supervised practice | Cillian O’Briain | Rehabilitation Subgroup | 31/3/26 |
| Motor Neurone Disease (MND) emotional wellbeing project | Follow on project focusing on exploring and enhancing emotional wellbeing pathways for MND | Cillian O’Briain | MND Steering Group | 01/12/26 |
| Multiple Sclerosis (MS) pathway development | Support improvements in GM MS pathway | Cillian O’Briain | MS Steering Group | 31/3/26 |
| Neurogenic Bladder and Bowel | Continue to support development of GM service | Cillian O’Briain | NR Inpatient & Community Forum | 31/03/26 |
| Oral suctioning | Work at GM level to ensure equitable access for patients in community | Cillian O’Briain | CNRT Forum | 30/12/25 |
| Out of Hospital Cardiac Arrest | Establish a model of care for patients presenting with hypoxia following cardiac arrest in GM. | Gemma Smith | NR Inpatient & Community Forum | 31/12/25 |
| Spasticity | Develop a robust, equitable pathway ensuring coordinated multi-disciplinary community spasticity services for all stroke/neuro patients. Support spasticity training and education of the GM workforce. Support the effective use of advanced roles | Gemma Smith | Rehabilitation Subgroup | 31/03/26 |
| Specialist equipment provision and IFR processes | Improve the GM specialist equipment provision pathways to create equitable access across localities. Work with ICB to improve IFR processes for seating and other areas | Cillian O’Briain/Gemma Smith | Rehabilitation Subgroup | 31/12/25 |
| Vestibular rehabilitation | Map current pathways across GM and identify service gaps. Develop a GM model for neurological vestibular service provision. Ensure workforce is appropriately competent to deliver assessment and rehabilitation. | Farheen Akhtar | Rehabilitation Subgroup | 31/10/25 |
| Workforce development | Coordinate Trust led introductory training for new starters and programme for experienced staff. Develop resources to support training and education of staff including posters and eLearning packages | Farheen Akhtar | Workforce Development Subgroup | Ongoing |
| Longer Term Support | ||||
| Longer Term Support: Stroke | Support implementation of the Integrated Life After Stroke Support model across GM. | Sarah Rickard | Stroke Inpatient & Community Forum | 30/12/25 |
| Longer Term Support: Neuro | Develop a model of longer term support for neurologically impaired patient across GM. Support implementation of model across GM. | Sarah Rickard | NR Inpatient & Community Forum | 30/12/25 |
| Patient & Carer involvement | ||||
| Empowering patients and carers | Empower people with Lived Experience to have increased influence over the work of the network | Sarah Rickard | Patient & Carer Group | Ongoing |
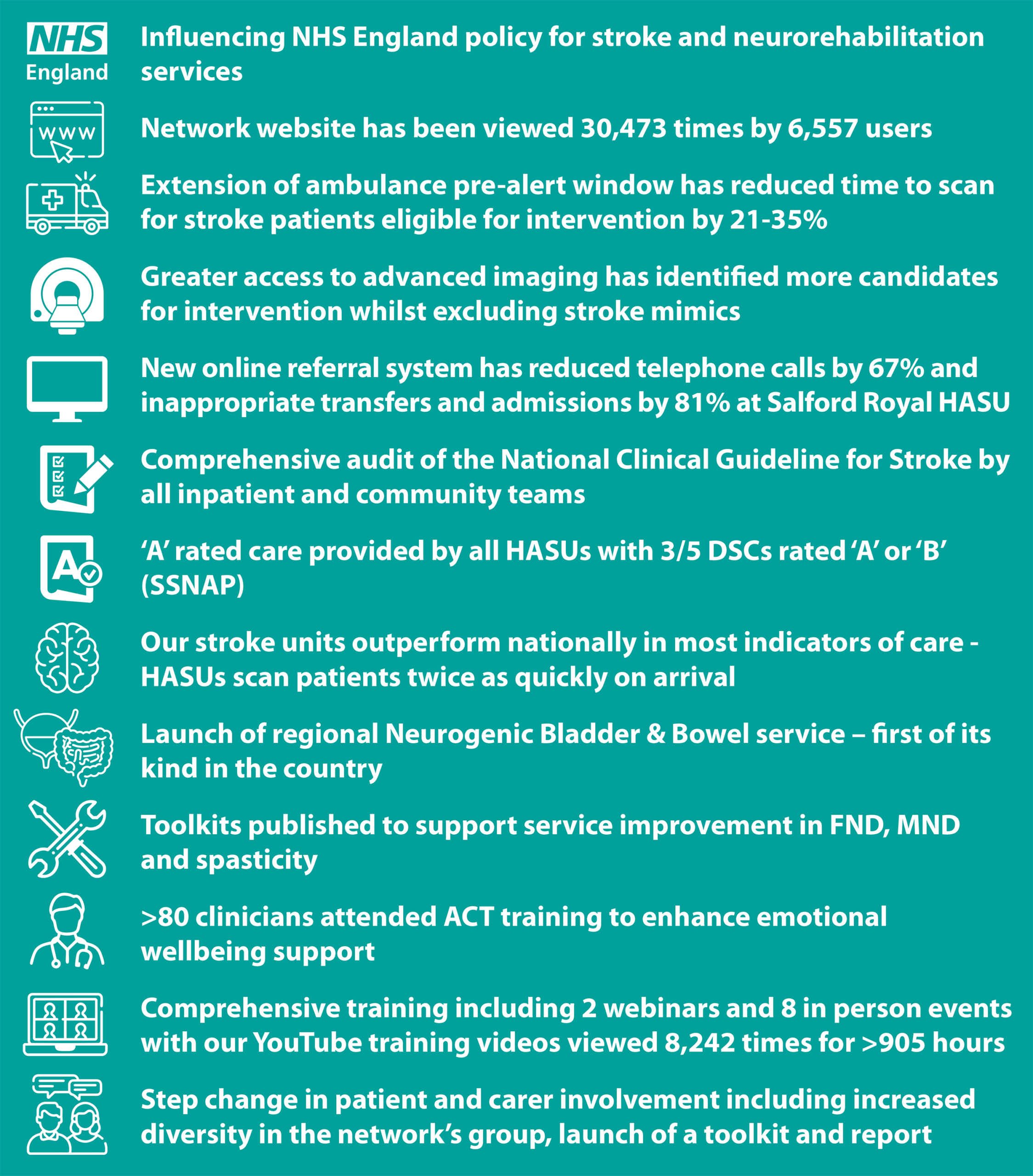
Impacts of our projects
It is important that our projects make a difference to the lives of patients and their families. Each project includes a range of measures that help determine their outcomes, outputs and impacts.
A summary of the impacts of projects completed in 2024/25 is below, with further examples highlighted in our annual reports.